Reasons of Helping

Hope and Dignity Restore
Every individual deserves to live with dignity and purpose. Many people living with mental illness face discrimination, isolation, and loss of self-worth. Through therapy, education, and community support, SMIF helps restore confidence and hope — empowering people to rediscover their value and live meaningful lives.
SMIF Nigeria
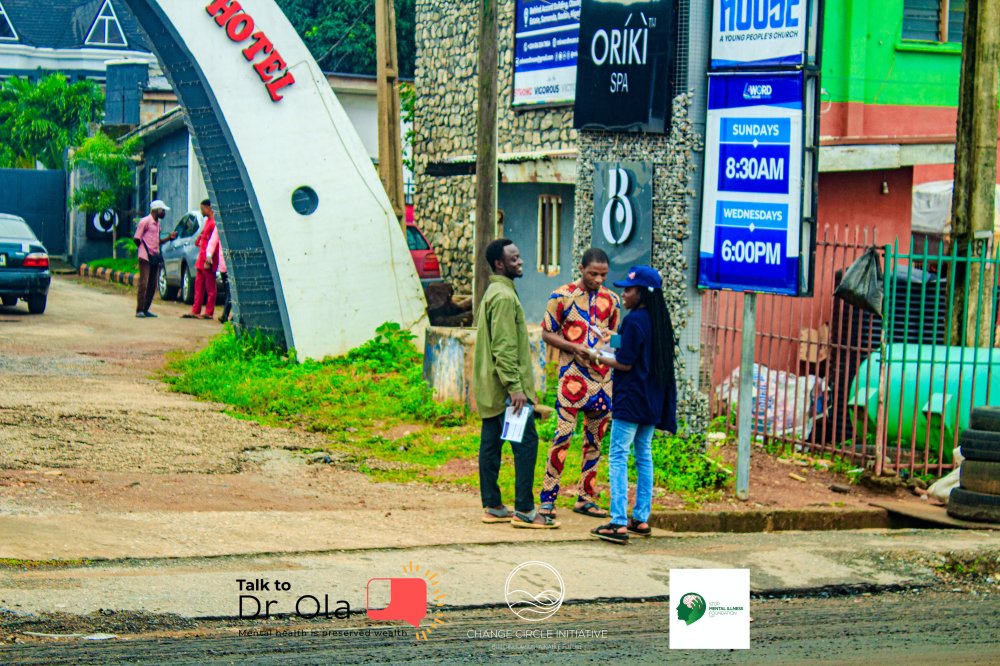
Mental Health Awareness and Early Intervention
Lack of knowledge about mental health often leads to late diagnosis and worsening conditions. SMIF is committed to spreading awareness, identifying early symptoms, and providing access to the right care and counselling. Early intervention saves lives and promotes lasting well-being.
SMIF Nigeria
Recovery and Sustainable Living
Beyond treatment, true healing includes empowerment. SMIF equips beneficiaries with life skills, vocational training, and community mentorship to help them achieve independence. By supporting SMIF, you help individuals rebuild their lives and contribute positively to society.
SMIF Nigeria